hEDS is a heritable connective tissue disorder that causes generalized joint hypermobility, joint instability, and chronic pain. hEDS is also associated with a variety of other symptoms and related conditions that affect many different areas of the body.
Hypermobile Ehlers-Danlos Syndrome (hEDS)
hEDS is the most common type of EDS, accounting for about 90% of EDS cases. hEDS is currently classified as a rare disorder and is thought to affect at least 1 in 3,100 – 5,000 people. However, the true prevalence of hEDS is not known and may be underestimated.
The cause(s) of hEDS have not been identified.
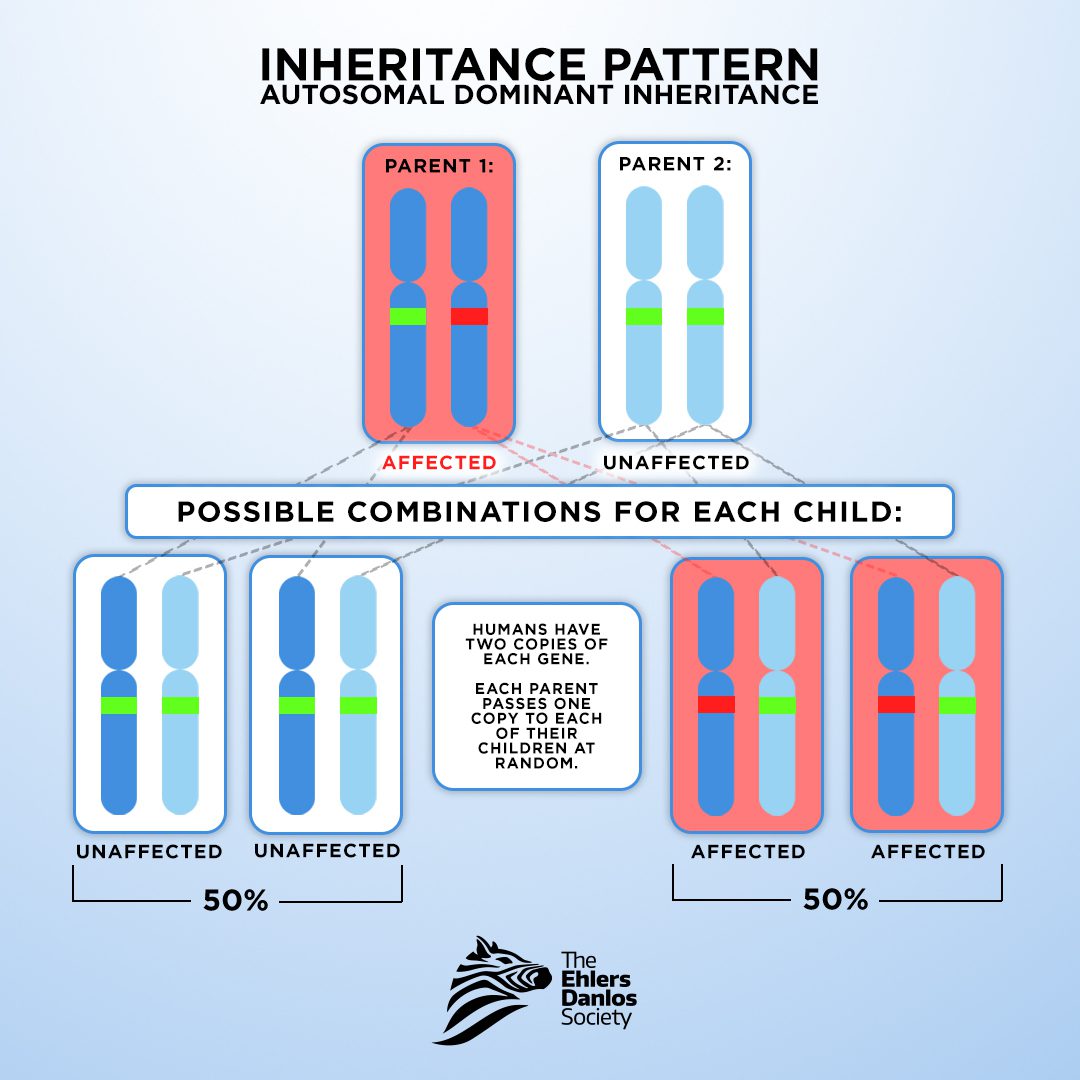
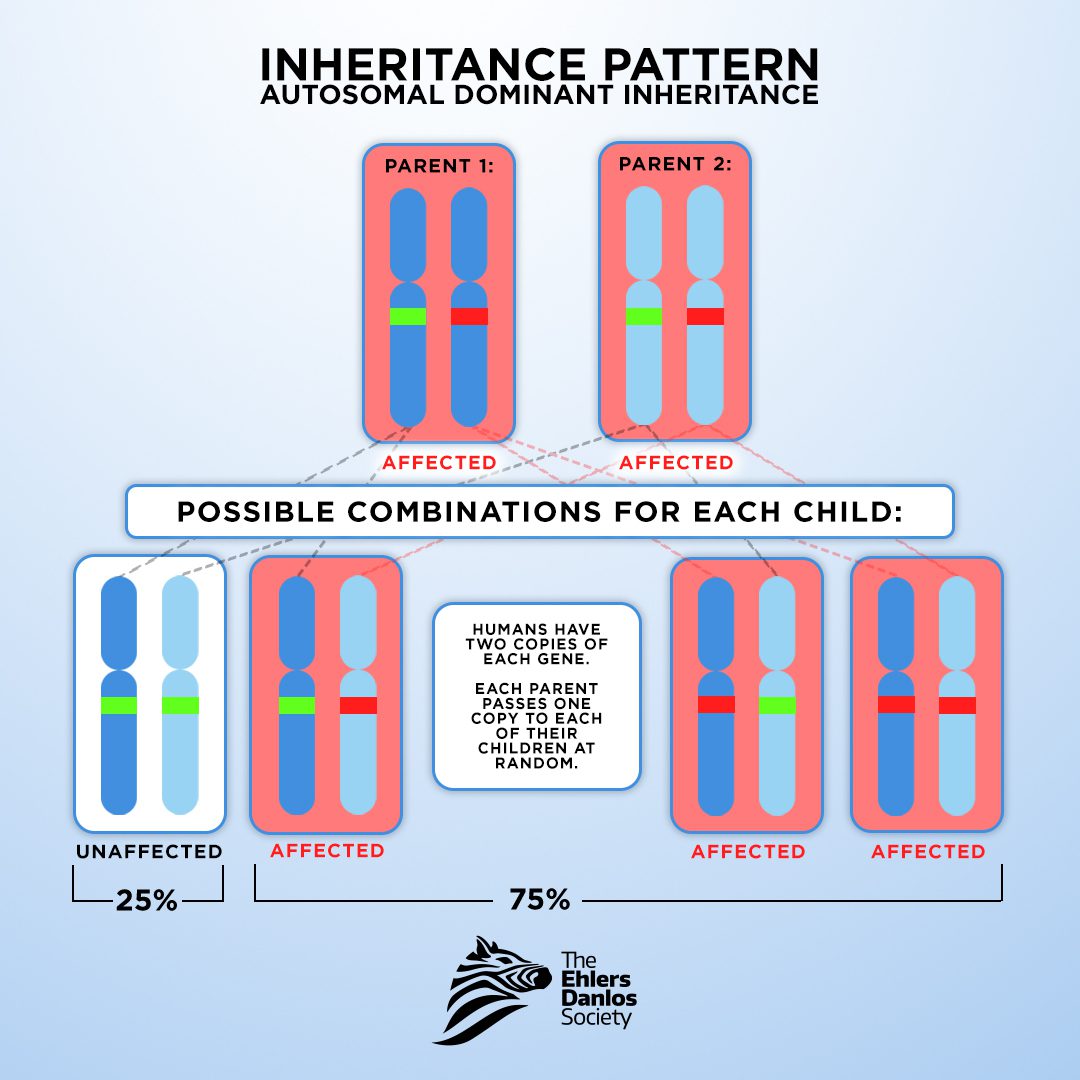
Though the cause(s) of hEDS have not been identified, the condition appears to follow an autosomal dominant inheritance pattern. This means each child of a parent with hEDS will have a 50% chance of having hEDS.
hEDS may be suspected if a person has:
- Joint hypermobility
- Joint instability
- Chronic pain
- Mild skin hyperextensibility
- Abnormal scarring
People with hEDS may also have:
- Chronic fatigue
- Gastrointestinal issues
- Dysautonomia
- Headaches
- Mast cell activation diseases
The cause(s) of hEDS have not been identified, so there is currently no laboratory test available to diagnose hEDS. The diagnosis of hEDS is given to those who meet the clinical diagnostic criteria for hEDS.
To meet the diagnostic criteria for hEDS, a person must meet all three criteria (1 and 2 and 3).
Criterion 1: Generalized joint hypermobility
Criterion 2: Two or more of the following features (A, B, and C) must be present
Feature A: Manifestations of a connective tissue disorder (must have five or more of the following):
- Unusually soft or velvety skin
- Mild skin hyperextensibility
- Unexplained striae such as striae distensae or rubrae at the back, groins, thighs, breasts, and/or abdomen in adolescents, men, or pre-pubertal women without a history of significant gain or loss of body fat or weight
- Bilateral piezogenic papules of the heel
- Recurrent or multiple abdominal hernia(s) (e.g., umbilical, inguinal, crural)
- Atrophic scarring involving at least two (2) sites and without the formation of truly papyraceous and/or hemosideric scars as seen in classical EDS
- Pelvic floor, rectal, and/or uterine prolapse in children, men or nulliparous women without a history of morbid obesity or other known predisposing medical condition
- Dental crowding and high or narrow palate
- Arachnodactyly, as defined in one or more of the following:
(I) positive wrist sign (Steinberg sign) on both sides
(II) positive thumb sign (Walker sign) on both sides - Arm span-to-height ratio ≥ 1.05
- Mitral valve prolapse (MVP) mild or greater based on strict echocardiographic criteria
- Aortic root dilatation with Z-score >+2
Feature B: Positive family history (one or more first-degree relatives independently meet the current diagnostic criteria for hEDS)
Feature C: Musculoskeletal complications (must have at least one of the following)
- Musculoskeletal pain in two or more limbs, recurring daily for at least three (3) months
- Chronic, widespread pain for at least three (3) months
- Recurrent joint dislocations or frank joint instability, in the absence of trauma (a or b)
(a) Three (3) or more atraumatic dislocations in the same joint or two (2) or more atraumatic dislocations in two (2) different joints occurring at different times
OR
(b) Medical confirmation of joint instability at two (2) or more sites not related to trauma
Criterion 3: ALL of the following prerequisites must be met:
- Absence of unusual skin fragility, which should prompt consideration of other types of EDS
- Exclusion of other heritable and acquired connective tissue disorders, including autoimmune rheumatologic conditions
- In patients with an acquired connective tissue disorder (e.g., lupus, rheumatoid arthritis, etc.), additional diagnosis of hEDS requires meeting both Features A and B of Criterion 2. Feature C of Criterion 2 (chronic pain and/or instability) cannot be counted towards a diagnosis of hEDS in this situation.
3. Exclusion of alternative diagnoses that may also include joint hypermobility by means of hypotonia and/or connective tissue laxity. Alternative diagnoses and diagnostic categories include, but are not limited to:
- Neuromuscular disorders (such as myopathic EDS and Bethlem myopathy)
- Other heritable connective tissue disorders (such as other types of EDS, Loeys–Dietz syndrome, Marfan syndrome)
- Skeletal dysplasias (such as osteogenesis imperfecta)
hEDS is managed by addressing the symptoms a person is experiencing. hEDS can cause a variety of symptoms in many different areas of the body, so people with hEDS may require multiple providers in different specialties to manage their care. Key aspects of care include physical therapy and pain management. Everyone with hEDS is different, so each person should work with their care team to develop a care plan that meets their individual needs.
The Ehlers-Danlos Society is funding a series of vital research studies to further the understanding of hypermobile Ehlers-Danlos syndrome (hEDS), with the goal of finding the underlying causes for these conditions, as well as developing diagnostic tests. Learn more.
